Two weeks before the 2025 Vermont legislature was about to adjourn in May, Representative Alyssa Black, a Democrat from Essex Town, attended an event at the State House featuring Middlebury students presenting on critical healthcare issues. As the sponsor of a major prescription drug bill hanging in the balance, she was hoping to learn something that might bolster its chances.
As it turned out, she found value in all eight of the poster board presentations by students in Professor Jessica Holmes’s Health Economics and Policy course, prompting her to walk straight back to her office to check on the date of Middlebury’s Commencement.
“They all presented valuable information on issues our committee was discussing so I wanted to see if I could get all of them back to testify to our committee before graduation,” said Black, chair of the House Committee on Health Care.
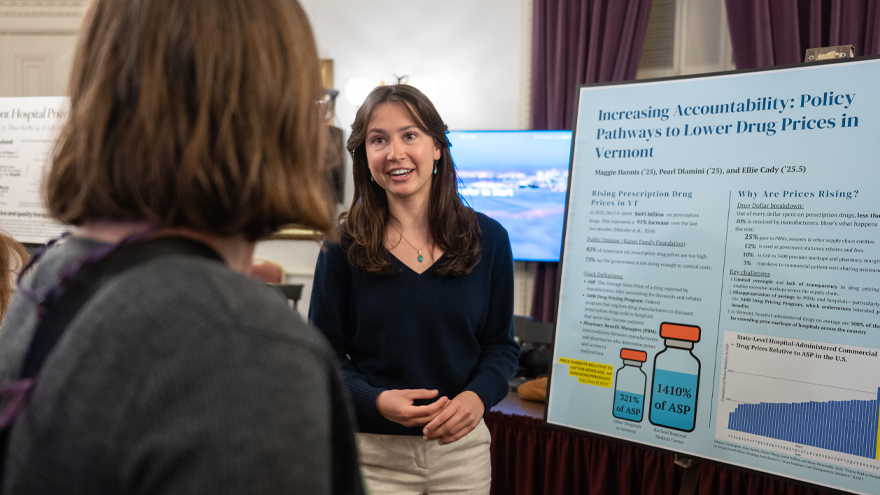
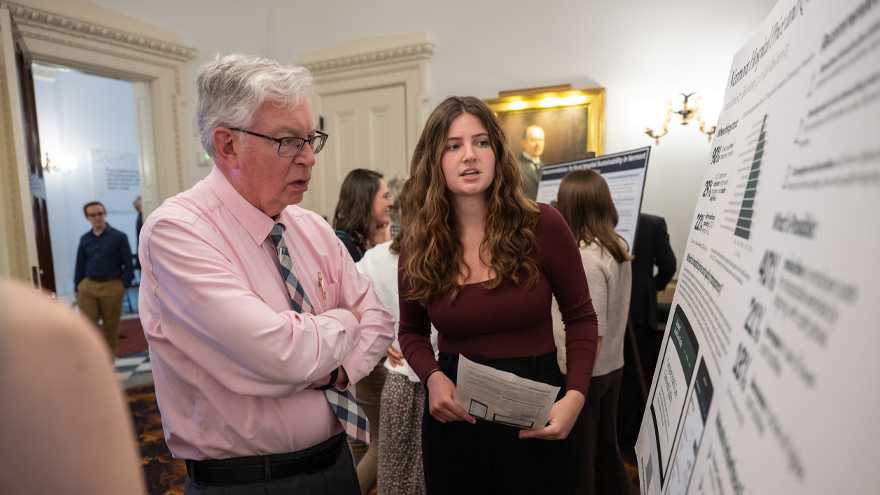
On May 14, six students worked around their finals schedule to testify before the House Committee on Health Care: Jonathan Brooks ’26 on the impact of private equity in health care; Elinor Keehn ’25, Sarah Holmes ’27, and Lily McGovern ’25 on Vermont hospital price and quality transparency; and Ellie Cady ’25.5 and Maggie Hannis ’25 on lowering prescription drug costs.
Black, who called the testimony the best her committee received, added an amendment to H.266 based in part on a proposal by Cady, Hannis, and Pearl Dlamini ’25 calling for a 120 percent cap on physician-administered drug prices. On May 28, the legislature passed the bill capping how much hospitals can charge for specialty drugs to treat cancers and autoimmune conditions.
Students based their recommendation on a RAND report and an analysis provided by Tom Weigel, MD, vice president and chief medical officer at Blue Cross and Blue Shield of Vermont, showing the state having the nation’s highest prices for outpatient pharmaceuticals.
“The students played a key role in moving this legislation forward,” said Weigel, who recommended the 120 percent cap to students. “Their research was sound, their communication was clear, and their presence at the State House came at exactly the right time. Policymakers listened—and I believe their work helped push this across the finish line.”
Creating Healthcare Experts
As professor and director of global health and a longtime member of the Green Mountain Care Board—an independent body appointed by the governor to improve healthcare quality and stabilize costs—Holmes is an expert on U.S. and state healthcare policy. She challenged her students to become experts as well by conducting literature reviews, analyzing policy models, interviewing experts, writing papers, and presenting to lawmakers.
“My goal was to give students a deep understanding of the U.S. healthcare sector and challenge them to develop evidence-based solutions to Vermont’s most pressing health policy issues,” said Holmes. “The timeline was short and the stakes were high. I am hard-pressed to think of a more realistic setting to hone essential skills in research, cold calling, collaboration, strategic thinking, and persuasive communication.”
Student teams of three chose the following eight healthcare challenges based on recommendations from legislators and the Green Mountain Care Board:
- Vermont Rural Hospital Sustainability
- Improving Healthcare Price and Quality Transparency in Vermont
- Reference-Based Pricing as a Potential Strategy to Lower Costs in Vermont
- Strategies to Lower Prescription Drug Costs in Vermont
- The Role of Private Equity in Health Care—What Does Vermont Need to Understand?
- Access to Primary Care in Vermont
- The Role of AI in Health Care
- Vermont Tax Policy to Improve Public Health (tax on alcohol, sugar, etc.)
The list of healthcare experts that students interviewed included presidents and CEOs of hospitals, and executives at the National Rural Health Association, Vermont Hospital Association, and Blue Cross and Blue Shield, as well as legislators, lobbyists, and consultants.
“I had some ideas I thought were going to be awesome, but then after talking with some of these people I realized it’s just not possible because of X,Y, and Z,” said Hope Shue ’25, a member of the rural hospital team. “It showed me the practical way the world actually works within an industry and legislatively. It also gave me hope as I enter the workforce next year that real human interaction and conversation is still necessary as opposed to just AI providing solutions to things.”
Mark Hage, member benefits director at the Vermont-National Education Association, appreciated the background knowledge students brought to his interview about reference-based pricing. “They explained the concept, applied it to Vermont, and argued why it was relevant to health care today and deserves serious consideration,” said Hage. “They covered both the empirical ground and the policy ground, and then bridged those two things together, which is always a challenge. They did their homework.”
Innovative Research
Students eventually started conducting their own research. The primary care access team became the first entity to call all 134 primary care and pediatric practices in Vermont—according to multiple legislators—to measure wait times. They conducted a “Secret Shopper Study” by calling for appointments and using GIS software to analyze disparities across Vermont’s 13 Health Service Areas. They found that 29 percent of practices were not accepting new patients; average wait times for new appointments were 62 days; and only 25 percent of voicemails were returned within four days.
“We have zero staff to do research so getting access to this level of information is incredibly helpful,” said Representative Edye Graning, a Democrat from Chittenden County, who expressed interest in students testifying before the House Committee on Commerce and Economic Development. “It’s a model that could work for other legislative issues. These are also workforce development issues.”
Elliott Fisher, a physician and professor of health policy at the Dartmouth Institute and the Geisel School of Medicine, included an informational slide from the primary care access group in a presentation he gave at the Rural Health Symposium: Advancing Rural Health Through Research, Policy, and Community Partnerships. “The students’ analysis of the remarkable variation in primary care access across practices in Vermont highlighted the current challenges in primary care access now confronting rural regions,” he said.
The rural hospital sustainability group developed a “hub-and-spoke model” centralizing complex care at well-resourced hospitals (hubs) and emergency and primary care at smaller hospitals (spokes)—integrated through shared services, data systems, and strategic planning. The reference-based pricing group developed an implementation plan for a payment strategy where the state would set pricing caps for healthcare services that are tied to Medicare reimbursements. The AI team recommended the creation of a statewide learning collaborative to encourage shared purchasing agreements to reduce costs and coordinate implementation. The price transparency group identified large price disparities between hospitals in Vermont and designed a prototype for a statewide price and quality shopping tool to help consumers make better informed healthcare decisions.
Presenting at the State House
Students arrived early on May 2 to set up their presentations in an ornate, stately room just off the main entrance of the State House. It wasn’t long before a mix of legislators, lobbyists, and healthcare professionals trickled in to watch students present and ask questions. “It was daunting at first to talk with them,” said Kelcey Dion ’25, “but it eventually got easier and they all seemed very approachable.”
Some student groups received pushback from lobbyists who disagreed with their policy recommendations. “The first person that came up told us that (our proposal) ‘was never going to work,’” said Janie Morganroth ’26. “I thought ‘oh my god, is this going to be the whole day?’ So it was a little scary at first but we grew more confident over time and other people told us that our ideas were great.”
Legislators appreciated the unbiased information. “We rely on a lot of advocates who are for or against issues, so getting neutral data like this is so important,” said Graning. “The presentations I looked at were right on target for what we are looking for in terms of objective information.”
Dan Olson, executive director of the Vermont Public Health Association, said students offered fresh perspectives. “This is amazing ammunition and more fodder for the discussion around the fact that we need more pre-education for volunteer legislators to elevate the discourse on these very complex policy topics.”
While some presentations touched on current healthcare issues, others provided a glimpse into the future. “Some of them touched on topics we aren’t really even thinking about yet,” said Representative Peter Conlon, a Democrat from Addison County. “Issues like AI and private equity are really important and will have an impact in Addison County. Hearing about what’s already happening in other states helps us get ahead of these issues.”
A week after the presentations, Holmes asked students to reflect on the course and State House experience. Some emphasized the importance of stepping out of their comfort zone to interview industry experts. Others said the course enhanced their critical thinking skills. For Cady, learning about the real-life circumstances of Vermonters struggling to pay exorbitant prices for life-saving drugs—then trying to craft a proposal to help them while not adversely impacting others—made it real.
“There aren’t a lot of classes like this that have real-life impacts,” she said. “Even after proposing a 120 percent cap on Vermont’s extremely high prescription drug prices, we struggled with the financial impact it might have on the ability of hospitals to continue providing certain services. There was a lot to consider. It felt real.”

Leave a Reply